Canada's national health-insurance program (also called medicare) is designed to ensure that every resident of Canada receives medical care and hospital treatment, the cost of which is paid through general taxes or through compulsory health-insurance premiums. Medicare developed in 2 stages. The first was the Hospital Insurance and Diagnostic Act of 1957, which gave the Canadian government authority to enter into an agreement with the provinces to establish a comprehensive, universal plan covering acute hospital care and laboratory and radiology diagnostic services. Nine years later, the Medical Care Act of 1966 extended health insurance to cover doctors' services.
While the basic principles of medicare are determined by federal legislation, responsibility for health under the Constitution falls under provincial jurisdiction. Therefore, there are certain variations in the plan from province to province. However, to be eligible for federal cost sharing, the provinces must in their health policies meet criteria of accessibility, universality, comprehensiveness, portability and administration.
Until 1977, federal contributions to acute hospital care and doctors' services matched provincial spending (approximately) dollar for dollar. At that time, unhappy that its share of health costs was in effect under provincial control, the federal government altered the arrangement by passing the Federal-Provincial Fiscal Arrangements and Established Programs Financing Act. Instead of 50-50 cost sharing, the federal government transferred to the provinces a lump sum based on a 3-year moving average of the Gross National Product and per capita cash payment.
The new arrangement allowed the provinces more flexibility, in that they were not limited to using federal funds only for insured hospital and medical services; federal money could now be applied to programs such as extended health care in nursing homes or drug-benefit plans not included in medicare. At this time, however, hospital costs were rising at a rate far exceeding general inflation, leaving the provinces with a heavier share of the health-cost burden. Matters worsened when, beginning in 1982, the federal government further restricted transfer payments.
History of Health Policy
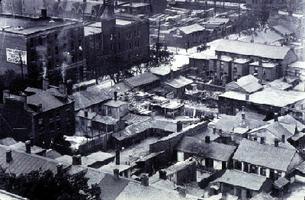
Prior to Confederation in 1867, there was little organized health care. Local communities had authority to set up their own health boards, and some did so in response to epidemics such as the cholera outbreak of 1832. The formal legislation authorizing such boards was passed by the Parliament of Upper Canada in 1834, but it was not until 50 years later that the Public Health Act compelled local governments to set up health boards and impose sanitary regulations. At meetings of the Canadian Medical Association, an organization created the same year as Confederation, doctors called for public-health measures, safe water and the reporting of contagious diseases.
Not until 1882 did Ontario legislation establish a provincial board of health. Three years later, with a smallpox epidemic raging in Québec, Ontario put public-health doctors on trains crossing the border into Ontario to inspect passengers; the doctors were empowered to arrest anybody who refused to be vaccinated.
Dental Care
Until the late 1800s there was a scarcity of dentists in Canada. Tooth decay among children was so prevalent that one Toronto dentist estimated that 50% of the schoolchildren at the turn of the century had rotten teeth. Today, provincial health-insurance plans provide some dental coverage, although such coverage varies from province to province, being generally limited to dental care in hospitals.
Some provinces, eg, Nova Scotia and Newfoundland, cover dental care for children, while Alberta provides coverage for citizens over 65. PEI has launched mobile child dentistry units staffed by salaried dentists. A study conducted in 1976 estimated that 18% of the population of Canada (ranging from a low of 3% in the Maritime provinces to 43% in BC) had some form of dental care provided through private insurers.
Mental Health
Under the Constitution Act of 1867, the provinces were made responsible for asylums for the mentally ill (see Mental Health). At that time, almost everywhere in the world the insane were kept at home or brutally treated. In Toronto, when a new and better jail was built in 1800, the old jail became an asylum. The Canadian National Committee for Mental Hygiene was founded in 1918, largely due to the efforts of Dr. Clarence M. Hincks, who with the help of leading Canadians raised funds for a survey of conditions in asylums across Canada.
These institutions were generally disgraceful, dirty and overcrowded. The committee brought this to the attention of the public, and the provinces soon began to spend more money on institutions for the mentally ill. By the 1950s, discoveries of drugs that could help control the behaviour of mental patients led to a new trend in care. Many patients from psychiatric hospitals were returned to the community. Prior to medicare, the only treatment available to the less affluent was in provincially owned psychiatric hospitals. Although the psychiatric care provided in general hospitals has greatly improved, the gaps in the continuum of care for the mentally ill are only beginning to be closed.
Health Insurance
The idea of health insurance had emerged in Germany in the late 1880s and spread throughout Europe, but social security programs were scarcely a priority in infant Canada. By WWI, Saskatchewan had created a plan under which municipalities could tax the population to build hospitals, hire doctors and pay for hospital care.
In 1919 the federal Liberal Party made a health plan a plank in its election campaign, but nothing came of it. During the Great Depression, the push for government assistance in meeting health-care costs gained momentum. People could not pay doctors' bills; indigents flooded the hospitals; municipalities, especially those on the Prairies, were bankrupt.
Prior to the enactment of a national hospital-insurance scheme, BC and Saskatchewan operated public, universal hospital-insurance plans. Alberta and Newfoundland had plans that provided partial coverage. By 1956, 50% of Canadians were covered by voluntary private or nonprofit prepayment plans, but public pressure for a nationwide program to protect people from catastrophic health-care costs was growing. This led to a federal government offer to share, on a grant-in-aid basis, the costs of a Canada-wide plan, on condition that the majority of provinces take part and a majority of the population be covered. By mid-1957, 8 provinces indicated that they would join in such a proposal. By 1961 all provinces had hospital plans in operation and 99% of the population was covered. This included coverage for all standard-ward hospital care.
Medical-services insurance was born, with considerable difficulty, in Saskatchewan in 1962. The Saskatchewan medical profession fiercely opposed the intentions of T.C. Douglas' provincial government to require doctors to collect their fees solely from the government plan. On July 1, 90% of the doctors closed their offices in protest (see Saskatchewan Doctors' Strike). The doctors won the right to bill patients if they so chose and to charge more than would be reimbursed to the patients under the provincial plan.
A year before the Saskatchewan battle, Prime Minister John Diefenbaker had appointed Justice Emmett Hall chairman of a royal commission on health services. In a 2-volume report (1964-65), Hall recommended medicare for all of Canada. In 1980 he was again asked to review the system, at which time he claimed it was, despite its problems, "by world standards one of the very best health services today."
Following the 1964 report, Prime Minister Lester Pearson promised that Canada would have a federal medicare program by 1967, and the necessary legislation was passed before the close of 1966. Not all provinces were eager to join the plan. A majority of Canadians were already insured under a variety of private or nonprofit plans, including a major one, Physicians Services Incorporated, run by doctors in Ontario. Nevertheless, by 1972 all the provinces and the territories had joined in.
Contrary to a widely held belief that doctors oppose medicare, the plan is supported by the Canadian Medical Association. Indeed the association itself proposed a national insurance plan in the 1940s. However, within the limits established by the federal Acts, each province has its own version of the plan. Some, such as BC and Ontario, pay to a limited extent for chiropractic services, optometry and physiotherapy, whereas Nova Scotia and Newfoundland do not. Saskatchewan and Manitoba pay for their plans from general revenues, whereas Alberta and Ontario charge insurance premiums for those who can pay. Some provinces also cover prescription-drug costs for senior citizens and social-assistance recipients.
Strike Action
Nevertheless, implementation of medicare by the provinces led to considerable tension between the provincial governments and provincial medical associations. Doctors feared, and still do, that medicare would become "state medicine," with governments the sole paymaster and doctors virtually civil servants. In 1986 the Ontario Medical Association opposed legislation (Bill 94) banning extra-billing by staging a 25-day strike, beginning June 12. Support for the strike action was not 100% within the medical profession itself and was almost nonexistent in the general population, and the doctors lost. The association called an end to the strike on July 6.
With extra-billing ended, Ontario recovered $106 million in federal funds, an amount equal to the sum doctors had billed patients directly in the preceding 2 years. The Ontario strike was the only major disruption of medical services in Canada since the Saskatchewan strike 24 years earlier, although medical specialists in Québec did withdraw their services for a short time when Québec implemented its plan in 1970.
The Québec plan is unique in that under it patients are not entitled to be reimbursed if they see doctors who bill patients directly. Thus, virtually all Québec doctors bill the plan and there is no extra billing. In August 1986 Alberta reached an agreement with its medical association to end extra-billing in that province, as did doctors in New Brunswick, without strikes.
Fears of State Medicine
Among Canadian doctors fears of state medicine escalated in the wake of the Hall Commission's 1980 report. The report cautioned that extra charges to patients (by 1984 Canadians were paying $70 million to physicians who extra-billed) constituted a barrier to accessibility to medical care that was contrary to the principle and spirit of medicare and that charges by doctors or hospitals would lead to a 2-tier health system, with different standards of care for those who could pay and those who could not.
Conflict among the various protagonists - the federal government, the provinces and the Canadian Medical Association (which represents the majority of Canada's 55 000 doctors) - was inevitable. The federal government claims that it contributes more than 50% ($12.2 billion) of medicare's costs by block grants to provinces and has sought to abolish extra charges to patients for insured services.
In 1983 it unveiled provisions designed to curb barriers to access and to eliminate extra billing. It requires that 100% of residents be entitled to insured health services, compared with 95% in previous legislation. The Canada Health Act provides for a reduction of the federal contribution to any province that does permit such patient charges by an amount equal, dollar for dollar, to the amount patients paid. The allied provincial and territorial health ministers deny that extra charges threaten medicare, claiming that the extra revenue is needed to supplement health funds in the face of rising costs and shrinking federal cost sharing. Each province allots roughly 33% of its budget to health.
The Canadian Medical Association claims that medicare is underfunded and that this has resulted in overcrowded hospitals, outdated equipment and waiting lists of patients requiring nonurgent surgery. The CMA estimated that 150 000 patients were on waiting lists in mid-1983 and the number has continued to increase. However, by 1986-87 there was a trend toward providing in the community and in patients' own homes medical care previously obtained in the hospital. New Brunswick, eg, pioneered a "hospital without walls" program. Treatments that once required patients be admitted to hospitals were provided in day-surgery units or out-patient clinics, reducing the need for more hospital beds.
Canada's medicare system compares well with health systems elsewhere in the world. Health-insurance administration costs in Canada were between 5% and 10% of expenditures, compared with over 10% in the US.

 Share on Facebook
Share on Facebook Share on X
Share on X Share by Email
Share by Email Share on Google Classroom
Share on Google Classroom

